Stents don’t work.
Editor's Note: Portions of this blog were originally published in 2017. Four years later and with more data the blog title still ring true - stents are not magic cures! Stents are an incomplete solution because they are a localized treatment…for a systemic disease. Lifestyle changes and especially improved nutrition are some of your best weapons at preventing and managing heart disease.
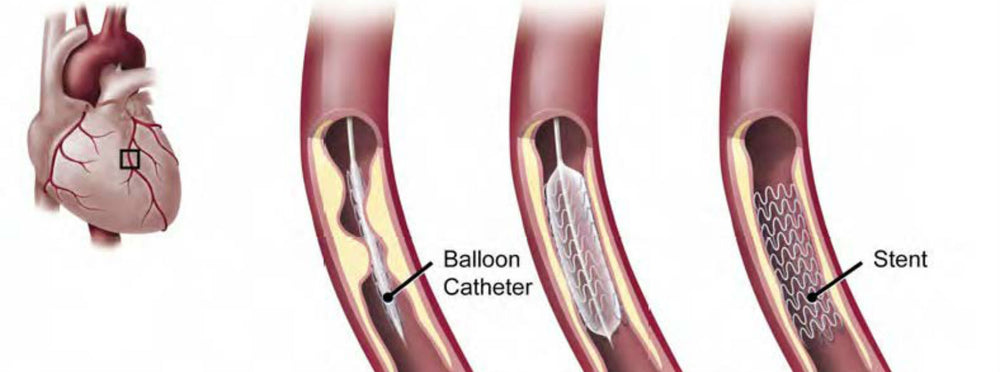
What are stents?
Stents have been used to open blocked heart arteries for decades. The first one was implanted in 1986 and use of stents quickly became commonplace. That’s because the little mesh devices, when expanded within arteries, are really good at keeping those arteries open. Inserting a stent costs between $11,000 and $41,000, and it’s estimated that at least 500,000 people undergo the procedure each year.
There is no question that stents can be lifesaving when they’re part of the treatment protocol for a heart attack. But most stents are not put in during heart attacks. Most stents are implanted because a blockage has been discovered after someone has been evaluated for angina (chest pain that occurs with exertion).
About The COURAGE Trial
At first, everyone – patients and doctors alike – were convinced that inserting stents in people with angina prevented future heart attacks. Turns out that’s not the case. A large study, called the COURAGE trial, published more than 10 years ago, found that there was no difference in the rates of subsequent heart attack, death or stroke between patients treated with stents as compared to those treated with medications alone.
But stents kept getting implanted. Because everyone – patients and doctors alike – were convinced that stents were really good at eliminating angina. Turns out that’s not the case either.
Another study – one that rocked the cardiology universe – found NO DIFFERENCE in chest pain relief among patients treated with stents compared to those undergoing a sham procedure.
The study was done in England and all patients were given drugs to reduce the risk of heart attack and prevent blood clots. Neither the patients nor the clinicians observing them during 6 weeks of post-procedure follow-up knew who got a stent and who didn’t.
Surprise Findings About Stents
And here’s the huge surprise finding – after 6 weeks, patients reported improvement in angina symptoms and demonstrated improved stress test results, regardless of whether they received a stent or not.
Study Results Without Stenting or Bypass
And now for the latest data validating this blog's title: About 7,000 patients with known coronary artery disease and stable angina were followed for an average of 5 years as part of a prospective registry. And guess what happened to these folks? Did they die? Did they require stent implantation? Did they all end up with bypass surgery? Nope. They simply got better over time!
- At one-year 40% saw their angina resolve.
- By 5 years, that proportion grew to 84% WITHOUT stenting or bypass!
- Only 4.5% of these patients ultimately required coronary artery stenting or bypass surgery because their condition worsened.
An important point: All of these folks were taking medications. More than 90% were on aspirin and cholesterol-lowering drugs and more than 70% were on additional heart drugs. Makes sense if you remember that coronary artery disease is one manifestation of a systemic illness. And medications like statins and other heart drugs affect the whole body - not just one area of blockage.
So Now What?
So are we all going to stop inserting stents now?
The chance that these results will change practice patterns is low. Because it's hard to not want to do SOMETHING if someone has a blockage - especially in an artery supplying blood to the heart! But all of these findings add up to a theme - and should truly give us pause as to how we treat heart disease today. Because pre-conceived notions about the effectiveness of our standard therapies just might be highly overblown, if not actually wrong.
What isn’t in dispute?
- A stent can save your life if you’re in the throes of a heart attack. This is probably where stents truly make the most difference and should be used.
- If you have coronary artery disease, sticking with prescribed medications (aspirin, statins, blood pressure lowering medications if you need them) is important. Remember, in all of these analyses, stents were compared to optimal medical therapy - not to no therapy.
- Lifestyle change – and especially a better diet - has been documented to reverse blockages, improve blood flow and help you avoid heart attacks. And help your medications work even better!

Tested & Proven Results.
- Cardiologist formulated
- Supported by over 500 publications
- Clinically-proven, in a double-blind randomized trial with Mayo Clinic and The University of Manitoba
80% of participants lowered their cholesterol in just 30 days. With just two servings per day, Step One Foods offers a proven-effective way to naturally lower LDL (bad) cholesterol.
Get heart health tips and articles like this, delivered right to your email.
New articles every week.
You may also like...

Insulin Resistance, Prediabetes and Type 2 Diabetes. Part 4: Un-Doing It.

You don’t need to avoid foods with cholesterol…except for these