Tips To Lower Your Cholesterol
Frequently Asked Questions
Here are some of the most frequently asked questions about cholesterol, and answers from preventive cardiologist and founder of Step One Foods, Dr. Elizabeth Klodas.
Want to learn more? See How To Lower Cholesterol or Statin Alternatives.
✅ Medically reviewed by Elizabeth Klodas, MD FACC
Last Updated: May 2022✅ Medically reviewed by Elizabeth Klodas, MD FACC
Last Updated: May 2022Cholesterol is a waxy fat-like substance that is absorbed from the intestines during digestion and is also manufactured internally by the liver - and by every cell in our body. The majority of cholesterol circulating in our blood and measured in a blood test does not come from the foods we eat but is rather manufactured internally. Cholesterol is a component of every cell wall of every organ and serves as a substrate for the formation of various hormones as well as bile (which helps us digest food). Cholesterol may be essential for various bodily functions but most of us have too much of it circulating in our bloodstreams.
High cholesterol has multiple potential causes including genetics, physical inactivity, excess weight and most importantly poor diet. In general, genetics alone are typically not the entire reason for high cholesterol. Even when people have genetically driven high cholesterol readings, other lifestyle factors usually coexist and make the numbers worse, sometimes markedly so.
According to the latest cholesterol management guidelines, fasting samples are not required for cholesterol testing and some clinicians even argue that a non-fasting sample is a more accurate picture of our cholesterol balance since we spend very little time during the day in a fasting state. However, all clinical trials that established cholesterol treatment goals were based on fasting measurements. In addition, triglyceride levels can vary substantially after a meal and since the formula used to calculate LDL includes triglycerides in the equation, LDL estimates may end up being off. Bottom line: If the cholesterol test is being used to help manage your medication dose or determine if you need to go on a medication in the first place, a fasting sample will be most accurate.
LDL is the Lousy cholesterol and we want to keep our LDL number Low. LDL or low-density lipoprotein is the form of cholesterol that can deposit in our arteries and cause blockages. This is the form of cholesterol that cardiologists obsess over and is the major target for cholesterol treatment. You can think of LDL as garbage. It’s what’s left over from other circulating cholesterol particles after the body has extracted all it needs from them. Because all our cells can make cholesterol internally, LDL does not serve much of a biologic purpose and it’s easy to see why high LDL levels could cause blockages to build up. That garbage has to pile up somewhere.
HDL is the Happy cholesterol and we want to keep our HDL number High. HDL or high-density lipoprotein is the form of cholesterol that is not depositing in our arteries but rather is on its way out. So we want as much of our total cholesterol in the HDL form. HDL cholesterol is also the cholesterol particle that is delivering cholesterol to various glands to be used in the formation of hormones. Although high HDL levels are felt to be protective against heart disease, this is not absolute which is why you can’t simply rely on a high HDL as being a guarantee against the risk of future heart events.
Foods high in cholesterol include eggs, shellfish, organ meats, fried and fast foods, processed meats, cheese, butter, etc. With the exception of shellfish, food-based cholesterol sources tend to be animal-based. But it’s not the cholesterol in food that is critical in determining blood cholesterol levels.
Triglycerides (TG) are fatty particles that transport excess calories around and don’t actually contain much cholesterol. If you recall, when we calculate LDL the formula has us divide the TG number by 5 to estimate the cholesterol contributed by triglycerides. TGs are not as much a risk factor for heart disease as they are an indicator of overall metabolic health. TGs also tend to be the most variable numbers in a cholesterol profile and, given their role in transporting calories around, are typically also most affected by nutrition status.
Triglycerides (TG) are fatty particles that transport excess calories. Normal TG levels fall under 150 mg/dL. But it’s important to know that TGs are measured on a completely different scale as compared to the other two cholesterol particles. The lowest TG level I’ve ever seen (in someone on no medications) is 27 mg/dL. The highest level was over 3000 mg/dL. So although everyone should be clustered under that 150 mg/dL mark, the possible range in values is huge. Relatively speaking, therefore, absolute changes in TGs are typically much less exciting than if the same changes were seen in LDL or HDL. Very high levels of triglycerides (especially those over 1000 mg/dL) are often genetically driven and raise the risk of pancreatitis (a painful inflammation of the pancreas, the organ that makes insulin and various digestive enzymes), so people with very high TG levels are typically placed on medications to prevent the occurrence of this condition. TGs are otherwise considered more of a secondary risk factor and are treated as part of the treatment plan for LDL.
Most people think that eating foods which contain cholesterol are the worst for raising blood cholesterol. That’s actually not the case. You’d have to gorge on a mound of plain shrimp to meaningfully move LDL, for example. It’s the overall composition of foods that really determines blood cholesterol levels - especially their saturated fat and simple carb contents.
Saturated fats are fats that are solid at room temperature. They come from animal sources and include fats from butter, cheese, the marbling in beef, the fat in chicken, and from egg yolks. Saturated fats are relatively neutral when it comes to HDL and TGs, but in some people can be very potent stimulants for raising LDL. Most recently, I have seen LDLs increasing dramatically during the keto diet craze, a dietary pattern which is very high in saturated fat content.
Simple, processed carbohydrates (think white foods like white breads buns and bagels, white rice, white pasta, white potatoes, cakes, cookies and other items made with added sugar and/or white flour) are also big stimulants for raising cholesterol.
Carbohydrates are naturally fat and cholesterol free so it's understandable why most people would not consider carbs a big driver of elevated blood cholesterol levels. But here’s where it gets complicated. All carbohydrates are absorbed as sugar. Simple/processed carbohydrates are easily digested and quickly absorbed causing blood sugars to spike. Which then causes insulin levels to spike. Insulin is a storage hormone and pushes our biochemistry into storage mode. What’s the storage form of cholesterol? LDL. LDL levels go up. What’s the non-storage form of cholesterol? HDL. HDL levels go down. What’s the storage form of sugar and excess calories? TGs. TG levels go up, often way up. End result? A pretty bad cholesterol profile.
Improving health - regardless of what you do to improve it - can help lower cholesterol. That includes exercising more, losing weight, reducing stress, stopping smoking, and improving diet. Of all those, improving diet has the greatest potential to reward you with the biggest cholesterol drops.
The main culprits are foods high in saturated fats and/or simple/processed carbohydrate. One obvious strategy for lowering cholesterol, therefore, is to avoid those foods. And that, for sure is essential – but sometimes people take this to the wrong extreme. For emphasis, eating to lower cholesterol does NOT mean eating a low fat or low carb diet! What it does mean is choosing healthy fats and healthy carbs instead.
Healthy fats are unsaturated, meaning they are liquid at room temperature. They come primarily from plant sources (as opposed to saturated fats that come from animal-based sources). Healthy fats include those found in olive oil, the oils in nuts and seeds, the oils in avocados and the oils in fish. These fats help lower LDL in most people. At worst they’re neutral in this regard. As a big bonus, unsaturated fats also help raise HDL and lower TGs.
Healthy carbs are complex/unprocessed carbs. In other words, carbs as close to their original form as possible. So steel-cut oats not a puffy oat cereal. An apple, not apple sauce or apple juice. Carbs in their most original form are the healthiest choice because they are difficult to digest - and are high in fiber and plant sterols. The “difficult to digest” part means that they are broken down and absorbed slowly, meaning blood sugar levels don’t spike. This means insulin levels don’t spike and you’re not placed into that counterproductive storage mode. In other words, by eating complex/unprocessed carbs you're helping to tamp down insulin release and avoid the simple carb-mediated rise in LDL levels.
To answer this, we first have to understand something about a natural cholesterol circulation system we all have in our bodies.
Every time we eat, a bunch of bile is squeezed into the digestive system to help digest the food we just consumed. Bile is very cholesterol rich. It’s one of the things we use circulating cholesterol to make. And we need a certain amount of bile always at the ready so we can digest food at any time. To keep that store of bile at adequate levels, we either need to pull cholesterol from the bloodstream to make bile for the next meal or reabsorb any bile not used up in the digestive process. The more bile we fail to reabsorb, the more circulating cholesterol we need to bring back to the liver to make bile for the next meal – which means circulating cholesterol levels drop. With me so far?
This is how the original cholesterol lowering drugs worked. They were called “bile acid resins” or “bile acid sequestrants” and they literally bound bile inside the digestive system so that you eliminated it through the stool. And these medications worked! LDL levels dropped! The problem was that bile sequestrants came as messy powders, you had to remember to take them with food, and they often caused stomach upset. So when statins came along, these medications were pushed to the sidelines. But that doesn’t mean the underlying biochemical pathways went away!
OK – we finally get to fiber. Fiber wastes bile because we can’t digest it. So you have a bile acid molecule attach itself to a fiber molecule and try to digest it. But before the bile figures out this is a futile mission, it’s past the point of no return. So people who eat diets high in fiber tend to waste more bile and therefore have lower cholesterol levels.
As an aside, fiber only comes from plants as part of a carbohydrate package. Meat and dairy do not contain fiber. This is why “low carb” diets (keto, paleo, Atkins, etc.) are often counterproductive to cholesterol management - especially once the weight loss levels off.
Plant sterols are also part and parcel of whole plants and are basically the plant versions of cholesterol. Which seems odd. Why would you eat cholesterol to lower cholesterol? We go back to that bile circulation process we just discussed. Plant sterols leverage the same biochemistry but in a different way. Plant sterols trick the body. They’re similar – but different – as compared to bile cholesterol. They’re similar enough that the body thinks those plant sterols are just like the bile cholesterol it needs to reabsorb. But because the sterols are just slightly different structurally, they can’t get through the bile absorption sites - and end up blocking them. This means bile has fewer spots through which to gain entry back into the body. And so we waste more bile. And LDL levels drop.
Cholesterol, especially LDL cholesterol, is highly correlated with heart disease risk. In fact, there is almost a linear relationship between LDL levels and the chance that someone develops plaque buildup – especially if LDL is elevated for a long time. Heart disease is multifactorial, so LDL can be more or less significant depending upon other risk factors, but in general, if your goal is to avoid developing heart disease (or avoiding additional events if you already have heart problems), the lower the LDL number the better.
That depends upon how you look at it. LDLs in mammals other than humans (who by the way share the exact same cholesterol pathways as we do), average between 30 and 55 mg/dL. When we’re born, our LDLs are also typically in this range. However, nearly all American adults would have to be on multiple drugs to get to these levels – so 30 to 50 mg/dL is probably an unrealistic benchmark.
Most cardiologists would say everyone’s LDL should definitely be below 130 mg/dL, with optimal levels falling below 100 mg/dL in otherwise healthy individuals. If you have known heart disease (like a history of heart attack stroke, bypass surgery, stent etc.) OR IF YOU HAVE DIABETES, your LDL should be closer to or below 70 mg/dL. Attaining LDLs below 50 mg/dL is additionally protective in terms of risk, and these levels are recommended in people who have had multiple cardiovascular events. As a reality check, people who live in Blue Zones (those areas around the globe where individuals experience exceptional healthy longevity), have average LDL levels around 90 mg/dL.
In short, no. Our cells have the capacity to make their own cholesterol, so there’s never a risk of running out of it. Some cholesterol is needed to make hormones but it’s typically HDL which is used for that purpose. Individuals genetically blessed with LDL levels in the 30s throughout their lifetimes do not experience any excess risk of any illness, cancer, dementia, etc. (and almost never develop heart disease). And they still have enough LDL to make bile for the next meal.
Not necessarily. If your total cholesterol is high and that’s only due to a high HDL, the elevated TOTAL cholesterol is much less worrisome. If your LDL is high and your HDL is high too, the negative impact of the high LDL might not be completely counterbalanced by the favorable HDL level. In general, we look at HDL and LDL as separate risk factors. When I run into this issue and it’s not clear that someone needs to be on statins, I will typically check a coronary calcium scan as the tie breaker.
Some physicians would say "yes" because of the known tight correlation between LDL levels and heart disease risk.
However, high cholesterol is only one risk factor and whether medication treatment is required needs to be considered within the context of the individual patient’s overall health circumstances. People who SHOULD be on statins include those with known atherosclerotic cardiovascular disease, those with diabetes and those with familial hypercholesterolemia (where LDL levels run over 190 mg/dL regardless of lifestyle factors). In everyone else, lifestyle efforts – and especially dietary adjustments - should be tried first. Consideration should also be given to checking a coronary calcium scan before starting statins in someone with elevated LDL who does NOT have heart disease, diabetes or familial hypercholesterolemia. This is what I do in my own practice.
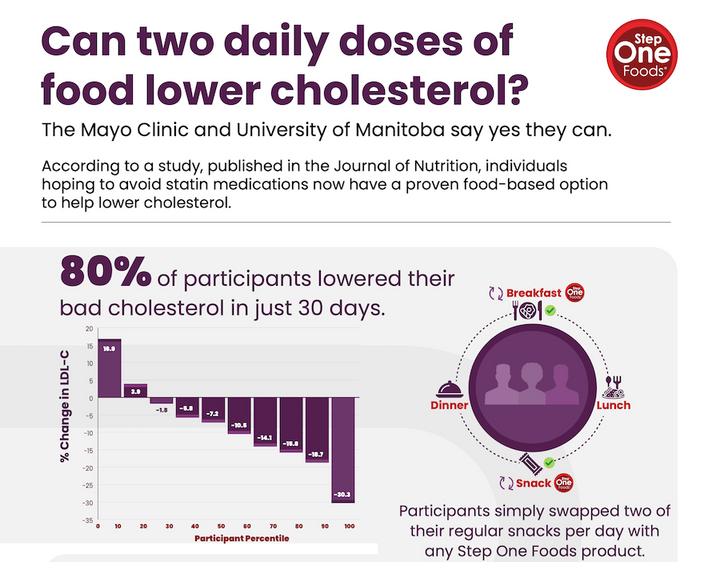
Medications can lower cholesterol almost instantly – you can see effects within days. But cholesterol levels can also change very quickly in response to diet. In studies where people were sequestered in laboratory settings and every morsel of food was controlled, LDL levels fell to their lowest attainable levels within 2 weeks! And we’ve demonstrated that even in a real world setting, using Step One Foods consistently can yield meaningful cholesterol reductions in most people after just 30 days.
This doesn’t mean you can’t have additional improvements over time. We are called “Step One” for a reason. Our products are meant to get you started and provide a simple and convenient foundation for your efforts, but losing weight (if you need to), getting more fit, and expanding your dietary efforts can yield even bigger improvements over time.
YES! It’s so common for people to think that because they take a medication to lower cholesterol they no longer need to pay attention to what they eat. But nothing could be further from the truth. If you eat in a way that supports lowering cholesterol, you will need lower doses of medications to get to your cholesterol goal. Your medications will also be more impactful in terms of lowering risk. Turns out, for any cholesterol reduction, risk is lower if the reduction was achieved with the COMBINATION of medications and diet. Finally, diet is not just important for cholesterol lowering. It’s also important for blood pressure control, blood sugar control and for weight loss (all of which are also risk factors for heart disease).
Want more? Here's how Step One Foods can Naturally lower bad cholesterol.